I've Seen MPOX!
In the early 2000s, I found myself in the middle of the first known U.S. Mpox, formerly known as Monkeypox, outbreak. I had a patient this week with lesions on their arms and legs. This made me realize I am one of the very few doctors in the entire United States who has actually seen Mpox on a human prior to our current outbreak.
The individual I encountered in 2003 had large, quarter-sized circular pits all over both of their arms. It turns out they were healing from Mpox due to a prairie dog exposure from a pet store. As a physician and a microbiologist, this grabbed my attention. I set out on a mission to find out everything there was to know about this disease. Much to my dismay, that didn’t go very far.
The CDC was, and still is, my go-to source for up-to-date and trusted microbial information. While they did verify the Mpox outbreak, there wasn’t much information available. At the time there didn’t seem to be human-to-human transmissions.
Forward 19 years to our current outbreak and now there is increasing human-to-human transmission. This is yet another example that we cannot become complacent with diseases that surround us. We need to study diseases coming from sources we, in the western world, may think we will never be exposed to. The more we intrude on the world’s forests and jungle regions; the more we travel “exotically”; the denser our population becomes; the more we risk furthering our exposures to these bugs enhancing their ability to mutate. This makes it all the more expedient to study and work together to prevent these diseases, even for decades as is evidenced here.
So what is Mpox anyway?
Mpox is a virus that is part of the smallpox family. It is not related to chickenpox. It causes a disease similar to smallpox but milder. Mpox first appeared in 1958 in research monkeys. These monkeys were in a lab in Denmark and not in the wild during their outbreaks. This led to it being named Monkeypox, which was changed in 2022 to Mpox by the World Health Organization. Later, blood samples of rodents in Africa also showed evidence of mpox.
The first human case wasn’t confirmed until 1970. The 2003 U.S. mpox outbreak was due to imported prairie dogs from Africa. So due to all of this information, it is thought the real source of mpox isn’t monkeys. That is just where it was first seen.

There have been outbreaks throughout the years in Africa. We now know that there was documented human-to-human transmission without noted mutations a decade apart. Outbreaks in the 1980s estimated that 30% were human-to-human transmission. This number jumped to 73% in the 1990s and the virus was not shown to have mutated between those outbreaks. Until 2003, Mpox appeared to be mostly isolated to the African continent.
Signs and symptoms
One to three weeks after exposure the patient may develop a fever, fatigue, cough, enlarged lymph nodes, cold symptoms, chills and body aches. Then one to three days after the fever starts they usually develop a papular rash anywhere on their body but it often starts on the arms, legs, face and groin area. This rash will increase to pustules that will crust and then dry up.
This process may last from two to four weeks. Some people will only develop the rash without prior symptoms. Other people will develop the symptoms after the rash. A patient is still infective to others until the rash has healed to the point that a new layer of skin has developed on the lesions.
How can I get Mpox?
From infected animals:
- by preparing or eating infected meat
- by bites or scratches from infected animals
- contact with an exposed pet
From bedding/clothes/materials that are contaminated by an infected person’s body fluids. This fluid may be semen, leakage from pustules, saliva, respiratory droplets and so on. Studies on this type of virus family have shown that it can live for weeks to months on surfaces in your environment. Bedding and clothing may hold the virus for longer periods due to its porous nature.
From Infected Human Contacts:
- close contact such as kissing or hugging
- any form of sexual contact or touching genitals
- respiratory droplets such as with prolonged face-to-face contact
- pregnant persons can transmit to the fetus
Infected persons can infect others from the onset of symptoms until the lesions have healed to the point of developing a new skin layer. This can go on for 4 weeks. It is also possible to transfer Mpox from a human to an animal such as a pet via the same routes.
How do I disinfect against Mpox?
In one case Mpox was still found in the patient’s home 15 days after the patient left the home. Other studies have shown this virus family can survive on surfaces for months. Household disinfectants and cleansing has been shown effective at removing the virus from the environment.
The following CDC recommendations should be followed:
- Use wet cleaning methods-dusting and sweeping may spread the virus into the air
- Pre-clean with soap and water, followed by an EPA-registered disinfectant. Follow its exact instructions for use.
- If you are not the infected person, wear gloves and masks at a minimum. Cover your entire body with clothing, cleanse the clothing immediately after cleaning and do not shake the clothing after removal.
- Cleanse all areas exposed to the infected person’s body and anywhere you have any doubt about exposure.
- Infected people isolated at home are suggested to regularly disinfect their home as well during their isolation.
- Practice regular hand hygiene with alcohol-based rubs and soap cleansing.

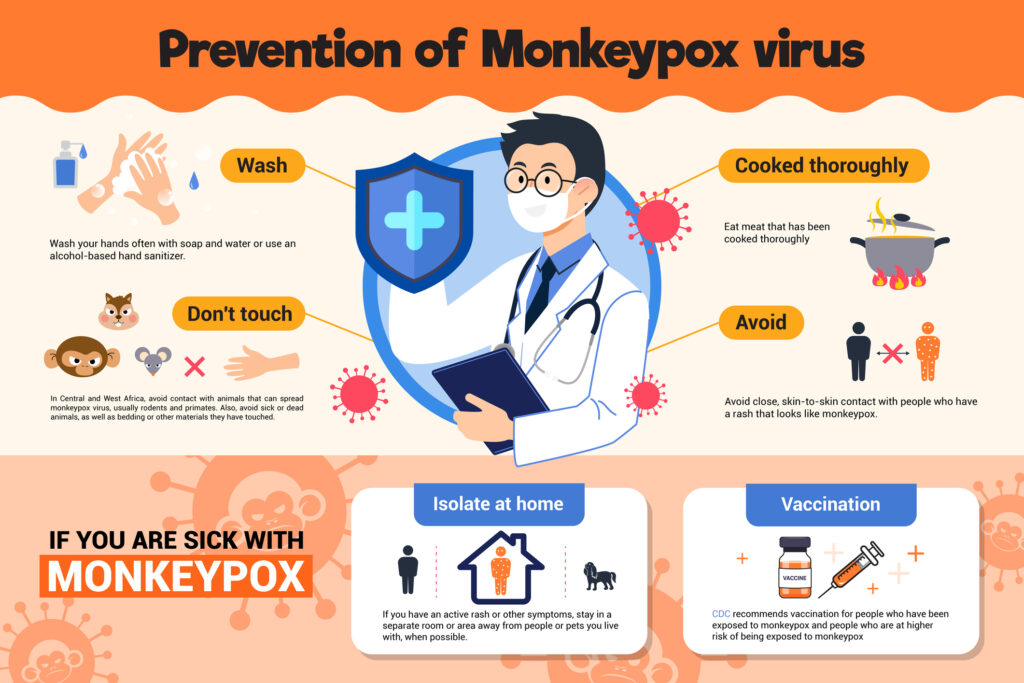
Preventing Mpox
- Practice safe sex!
- Get vaccinated—The CDC recommends the vaccine for people who have been exposed to Monkeypox and those that are at an increased risk of contracting Mpox.
- Avoid exposed persons, exposed animals or pets, and infected animals or persons for at least four weeks.
- Practice environmental and personal hygiene.
How is Mpox treated?
There is currently no treatment for Mpox. There is a vaccine for Monkeypox, Jynneos, that is being administered to those deemed at risk. Some states are administering the Mpox vaccine to those infected or those exposed to Mpox.
A smallpox antiviral medication called TCOXX is being used in some instances, as Mpox and smallpox are similar. Some state health boards recommend it for persons who are infected with Mpox and less than 8 years old, pregnant, immunosuppressed (e.g., AIDS, cancer, etc.) or have certain skin conditions such as eczema. Please call your local health department immediately if you or someone you know thinks they have been exposed to or have symptoms of Mpox.
Seminar Pediatric Infectious Disease 2004 October, NCBI/NIH website, PubMed Central, accessed August 2022
Centers for Disease Control and Prevention/Monkeypox July 2022, CDC website, US government, accessed August 2022
Mississippi State Department of Health/Monkeypox 4 August 2022, MSDH government website, accessed August 2022
